Health and Human Services
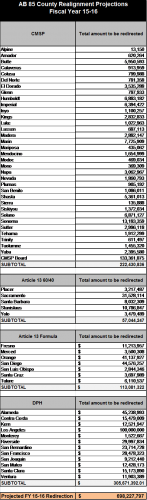
AB 85 Updated County-By-County Diversion Amounts
Below are the updated county-by-county diversion estimates. The original estimates published in our January 16 bulletin did not accurately reflect the jurisdictional risk amounts for the CMSP counties. This has been corrected. Please note that all county estimates will be updated during the May Revise.
California’s Health Homes for Patients with Complex Needs (HHPCN) Proposal
Section 2703 of the Affordable Care Act of 2010 grants states the ability to create an optional Medicaid Health Home benefit that provides a comprehensive system of care coordination for individuals with chronic conditions. The Health Home benefit does not fund direct medical or social services, but instead includes a package of six care coordination services:
- Comprehensive care management
- Care coordination
- Health promotion
- Comprehensive transitional care/follow-up
- Patient and family support
- Referrals to community and social support services
These services would be provided to a target population chosen by the state from one or more of the following categories:
- Two or more chronic conditions;
- One chronic condition and at risk for a second; and/or
- A serious and persistent mental health condition.
Assembly Bill 361 (Chapter 642, Statutes of 2013) authored by Senator Holly Mitchell during her time in the Assembly, is California’s authorizing Health Home legislation. AB 361 authorized the Department of Health Care Services (DHCS) to create a Health Home program for Medi-Cal enrollees with chronic conditions, subject to federal approval.
In November 2014 DHCS released their health homes concept paper in conjunction with hosting a webinar. DHCS outline several key elements of their health homes proposal with other elements still to be developed. Key elements include:
Eligibility . DHCS proposes to target the three federal categories as outlined above, with an emphasis on persons with high costs, high risks and high utilization who can benefit from increased care coordination of physical health, behavioral health, community-based long term services and supports and social supports resulting in reduced hospitalizations, emergency department visits, improved patient engagement and decreased costs.
The state also envisions rolling out Health Homes in a phased approach, starting with counties participating in the Coordinated Care Initiative (CCI) – Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo and Santa Clara. DHCS believes that as a result of preparing for the CCI, the Medi-Cal managed care plans in the CCI counties are more likely to have the infrastructure and experience to implement the Health Home program. The plans in CCI counties would implement in January 2016, and plans in other counties would implement six months later. During the Stakeholder Advisory Group meeting on February 11, DHCS stated that they are willing to include non-CCI counties in the first phase of the roll out as the county’s readiness allows. Each phased in county roll-out would require a new state plan amendment (SPA), which would allow eight quarters of 90% federal financial participation for counties included in the SPA.
Health Home Network Infrastructure . DHCS is proposing a health home network with 1) lead entities; 2) community-based care management entities; and 3) community and social support services.
- Lead Entity . DHCS designated qualifying Medi-Cal managed care plans as the lead entity with the responsibility for the entire health home network. This includes receiving the health home payment from the state and passing funds to the partnering entities.
Lead entities must demonstrate the ability to:
- Assemble the overall health home network;
- Administer and be accountable for the health home network;
- Collect, analyze and report on financial, health status and performance measures; and
- Connect enrollees to a care management entity and dedicated care manager.
- Community-Based Care Management Entities . Community-based care management entities could include federally qualified health centers, hospitals, clinics, independent provider associations and behavioral health partners. These entities would contract with the plans to provide the core health home services and would provide payments from the plan.
A community-based care management entity must demonstrate the ability to:
- Actively engage enrollees in developing, reinforcing and supporting their health action plan;
- Coordinate physical health, behavioral health and community-based long-term supports and services with other providers;
- Advocate for and educate enrollees to attain and improve self-management skills; and
- Ensure the receipt of evidence based care.
- Community and Social Supports . Community and social supports could include housing providers, food banks, employment assistance, and social services agencies that provide services to meet the enrollees’ broader needs, but may not necessarily receive health home funding.
Services . States must provide the six core services, yet have the authority to define each of them. Currently core definitions are defined by DHCS as follows:
- Comprehensive care management – primarily involves activities related to developing the enrollees’ comprehensive, individualized care plan, called a health action plan.
- Care Coordination and Health promotion – includes the implementation of the enrollees’ health actin plan.
- Comprehensive Transitional Care – addresses the activities related to preventing patient admissions and readmissions.
- Individual and Family Support Services – includes activities that ensure the enrollee and their family are knowledgeable about the enrollee’s conditions to improve the enrollee’s adherence to treatment.
- Referral to Community and Social Supports – addresses the identification of community-based resources to refer the enrollee to. This includes an active referral and follow-up as necessary.
- Use of Health Information Technology and Exchange to Link Services – still being developed.
Payment Methodology . Per DHCS, the payment method will likely be “a per member per month” (PMPM) carved into the managed care capitation payment. DHCS also intends to create payment tiers based on patient acuity and the intensity of service needs. Payment would be flow from DHCS to the lead entity (the qualified managed care plans), who would pass payments to the care management entities via contracts. DHCS intends to further develop this concept.
Next Steps . There is much work still to be done as DHCS is aiming to submit a State Plan Amendment (SPA) in August 2015 and to implement in January 2016. Additionally, DHCS will be releasing a revised concept paper in conjunction with a stakeholder engagement event in March 2015. They will also continue to host stakeholder events between March and the SPA submission in August to solicit feedback as their proposal develops.
DHCS is still soliciting reactions to their November concept paper, which will inform their March concept paper. The November concept paper and other health home materials can be found on the DHCS webpage at: http://www.dhcs.ca.gov/provgovpart/Pages/HealthHomes.aspx.
CSAC will continue to provide updates as additional details are made available.
Bills
SB 196 (Hancock) – Pending
As Introduced on February 10, 2015
Senate Bill 196, by Senator Hancock, would authorize a county adult protective services agency to file a petition for a protective order on behalf of an elder or dependent adult if the elder or dependent adult has been identified as lacking the capacity to do so and conservatorship is being sought. Current law authorizes the following persons to seek an order: a conservator or trustee, an attorney-in-fact, a person appointed as a guardian ad litem, or other person legally authorized to seek the order. SB 196 seeks to add a county adult protective services agency as an authorized entity.
SB 196 is sponsored by the County Welfare Director’s Association of California.
AB 253 (Hernández) – Pending
As Introduced on February 9, 2015
Assembly Bill 253, by Assembly Member Roger Hernández, is currently a spot bill stating the intent of the Legislature to enact legislation to ensure the appropriate oversight mechanisms are in place to capture best practices at the county level to ensure veterans have access to services provided by the Mental Health Services Act.
This bill comes on the heels of the Little Hoover Commission’s Report on the Mental Health Services Act as reported in CSAC’s January 30 bulletin.
CSAC will closely monitor this bill and others related to MHSA.